Men, addiction, and trauma
Trauma is a profound emotional response to events that shatter one’s sense of security, leading to feelings of helplessness, vulnerability, and a variety of stress-related symptoms. While trauma can arise from obvious sources like warfare or natural disasters, it can also stem from personal experiences such as accidents, abuse, or sudden loss. Men often face overwhelming emotions and memories that can persist long after the event, impacting their mental health, relationships, and daily functioning. Often, this can lead to increased substance use, with about 75% of men with a substance abuse problem having experienced trauma at some point in their life. Trauma and addiction are deeply interconnected challenges that often co-occur in individuals, especially men, across various stages of their lives.

Trauma's Impact on the Brain and Body
Trauma can profoundly impact both the brain and body, leading to a variety of physiological and psychological effects. Trauma can alter the brain’s structure and function, particularly areas like the amygdala (fear response) and hippocampus (memory processing). The body’s response to trauma also includes an increased release of stress hormones like cortisol, all of which can lead to the following impacts of trauma:
- Anxiety and Fear: Intense and overwhelming feelings of anxiety or fear that are disproportionate to the current situation. For example, someone might feel panicked during a thunderstorm because it reminds them of loud noises associated with a traumatic event.
- Intrusive Thoughts: Unwanted and recurrent thoughts about the trauma, which can surface without any apparent trigger. For instance, a person who survived a car accident may repeatedly visualize the crash even while in unrelated settings.
- Mood Swings: Sudden, dramatic changes in mood, such as feeling fine one moment and overwhelmingly sad the next. For example, someone may start the day feeling upbeat but suddenly feel despondent without a clear reason.
- Irritability and Anger: An increased tendency to feel anger or irritability. This might manifest in situations where the individual feels out of control or overwhelmed, leading to short tempers or aggressive behaviors. For example, a war veteran may become irritable when loud noises disrupt their sense of control.
- Flashbacks: Vivid, distressing memories of the event that make a person feel like they are reliving the traumatic experience. A veteran, for example, might experience flashbacks during fireworks that make them feel like they are back in a combat zone.
- Sleep Disturbances: Difficulties in falling or staying asleep, nightmares, or experiencing terror at night, often related to fears stemming from the trauma. For instance, a victim of a home invasion may have trouble sleeping or experience nightmares about the event.
- Hypervigilance: An enhanced state of sensory sensitivity accompanied by intense behaviors with a purpose to detect threats. Hypervigilance can be triggered by environments that resemble the traumatic setting. For example, a person who was attacked in a dark alley might feel on edge when walking through similar areas.
- Startling Easily: A heightened startle reaction to unexpected noises or surprises, which may be a direct response to feeling constantly on edge or anxious. For example, a car backfiring might cause a disproportionate jump or scare in someone with trauma.
- Avoidance: Deliberately avoiding places, people, or activities that remind them of the trauma, which can affect personal relationships and social activities. For example, someone who experienced a traumatic event in a crowded market may avoid going to any busy public places to prevent the reliving of traumatic memories.
- Withdrawal: Pulling back from social interactions and activities, often as a way to avoid triggers or out of a fear of experiencing anxiety or other distressing emotions. This might include skipping gatherings or being unusually quiet in social situations.
- Loss of Interest: Decreased interest in significant activities, including hobbies, work, or socialization. For instance, a person who used to enjoy photography might lose interest after witnessing a traumatic event through their lens.
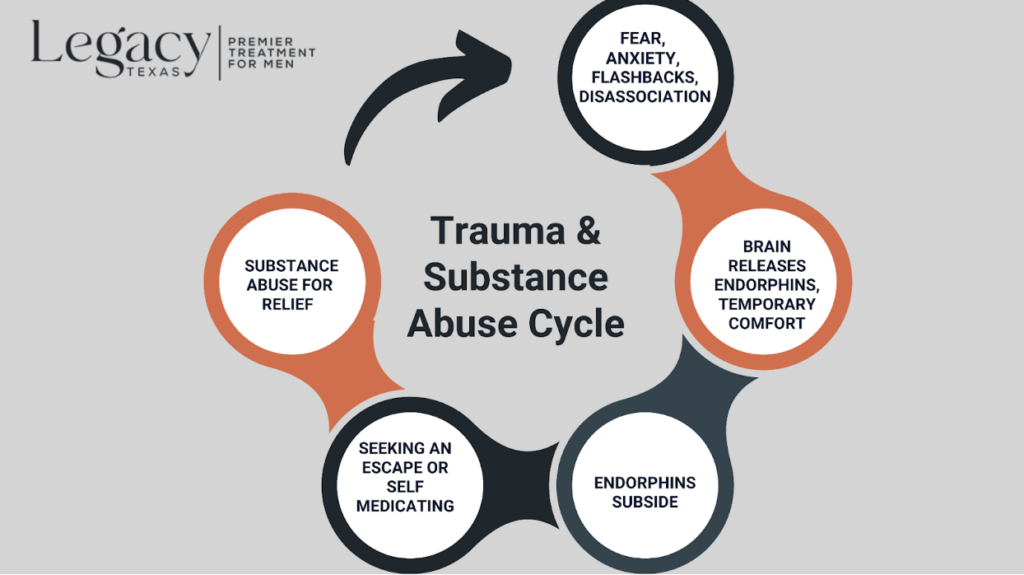
The Connection Between Trauma and Addiction
Unfortunately, men often use substances as a coping mechanism to self medicate and try to handle the distressing symptoms of trauma. In fact, research has found that men diagnosed with post traumatic stress disorder (PTSD) are twice as likely to abuse alcohol and 3x as likely to abuse drugs than men without trauma. Using substances to manage symptoms may provide initial, temporary relief, but this often begins a cycle of habitual use, increasing the risk of developing an addiction as tolerance builds and withdrawal symptoms emerge.
Signs and Symptoms of Addiction in Men
When trauma and addiction intersect, the signs and symptoms can manifest in complex and overlapping ways, intensifying previous symptoms experienced by trauma. Heightened symptoms experienced commonly include:
- Mood fluctuations
- Anxiety and paranoia
- Flashbacks and nightmares
- Irritability and anger
- Withdrawal from social activities
- Increased sensitivity to stress
- Physical tension
- Impulsive or risky behaviors
- Concentration problems
- Emotional numbness
- Changes in appetite or sleep patterns
These symptoms can create a reinforcing cycle where trauma exacerbates substance use, and substance use intensifies the symptoms of trauma, making it crucial to address both issues simultaneously in treatment.
Professional Treatments and Self-Help Strategies
Due to societal expectations and stigma for men to be strong and self-reliant, men are often less likely to seek professional treatment for trauma and addiction. This causes them to try to cope on their own terms, often trying to numb the feelings and pain the trauma has caused, increasing likelihood of addiction. Substance abuse can go unnoticed for years, exacerbating the trauma and addiction cycle. Addressing both trauma and addiction requires a comprehensive approach that includes professional evidence-based treatments and practicing self care strategies that become a regular part of life.
Professional Treatments
- Cognitive Behavioral Therapy (CBT): Focuses on changing negative thought patterns and behaviors associated with trauma and addiction.
- Dialectical Behavioral Therapy (DBT): Teaches patients skills in four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
- Prolonged Exposure Therapy: Helps patients confront and gradually process traumatic memories to reduce their psychological impact.
- Eye Movement Desensitization and Reprocessing (EMDR): Utilizes eye movements to help process and make sense of traumatic memories.
- Dual Diagnosis Treatment: Addresses both mental health issues like PTSD and substance use disorders simultaneously.
- Group Therapy: Provides support and perspective through shared experiences and peer feedback.
Self-Help Strategies
- Rebuilding Physical and Mental Strength
- Understanding and Reflecting on Your Past
- Practicing Mindfulness and Meditation
- Creating a Structured Daily Routine
- Eating Healthy Foods
- Prioritizing Sleep and Hygiene
- Cultivating Discipline and Resilience
- Joining a Supportive Community
Combining these research-backed treatments and personal self-help habits can significantly enhance recovery outcomes by addressing the connected challenges of trauma and addiction.
How Legacy Texas Can Help
Legacy Texas integrates holistic approaches with evidence-based treatments, providing a supportive environment where men can focus on healing and reclaiming control over their lives and legacies. By addressing the link between trauma and addiction in men, we create a path toward lifelong recovery that respects the mental health challenges commonly faced by men. At Legacy Texas, reclaimed history meets wellness. Reach out to us today to learn more about our program today!
Create a legacy you're proud of
Contact Us